Ureteric Stricture
Understanding Ureteral Stricture: Causes, Symptoms, and Treatment
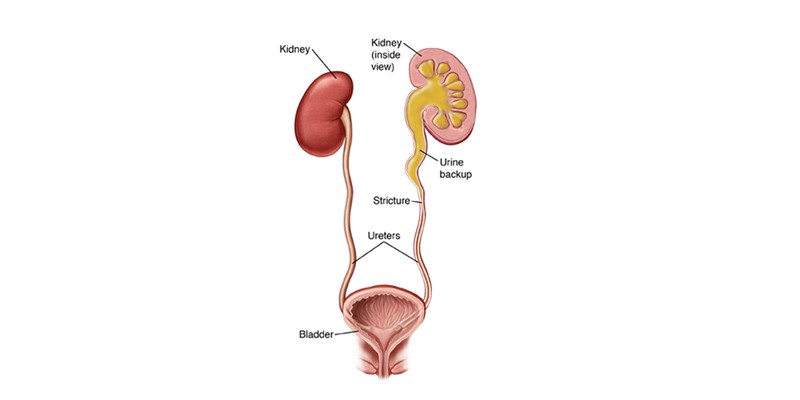
A ureteral stricture is a narrowing of the ureter, the tube that carries urine from the kidneys to the bladder. This condition can obstruct the normal flow of urine, leading to discomfort and potential complications if left untreated. Ureteral strictures can develop due to various causes and may present with a range of symptoms, requiring timely diagnosis and intervention.
What Causes Ureteral Stricture?
Ureteral strictures can arise from a variety of factors, including:
- Trauma: Injuries to the ureter, whether from accidents or surgical procedures, can lead to scarring and narrowing.
- Infections: Chronic or severe urinary tract infections (UTIs) can cause inflammation and subsequent scarring.
- Kidney Stones: Stones lodged in the ureter can damage the lining and create strictures.
- Congenital Conditions: Some individuals are born with structural abnormalities that predispose them to strictures.
- Tumors: Growths in or around the ureter can compress or invade the structure, leading to narrowing.
- Radiation Therapy: Treatment for cancers in the pelvic region can damage ureteral tissue, causing strictures over time.
- Iatrogenic Causes: Medical interventions, such as the placement of stents or catheters, can sometimes result in scarring and stricture formation.
Symptoms of Ureteral Stricture
The symptoms of ureteral strictures vary depending on the severity of the obstruction. Common signs include:
- Pain: Flank pain or discomfort in the lower abdomen may occur due to blocked urine flow.
- Urinary Changes: Difficulty urinating, decreased urine output, or a weak stream are common.
- Blood in Urine (Hematuria): This can occur due to irritation or damage in the ureter.
- Recurrent Infections: Frequent UTIs may signal an underlying obstruction.
- Kidney Swelling (Hydronephrosis): Prolonged obstruction can lead to fluid buildup in the kidney, potentially causing damage.
- Nausea and Vomiting: These symptoms may arise from severe urinary retention or kidney issues.
Diagnosis
Diagnosing ureteral strictures involves a combination of clinical evaluation and diagnostic tests:
- Medical History and Physical Exam: Understanding symptoms and past medical interventions helps identify potential causes.
- Imaging Studies: Ultrasound, CT scans, or MRI provide detailed visuals of the urinary tract and detect blockages.
- Retrograde Pyelography: This specialized X-ray involves injecting contrast dye into the ureter to outline the stricture.
- Ureteroscopy: A thin, flexible scope inserted through the urethra allows direct visualization of the stricture.
- Urine Tests: These can detect infections or the presence of blood that may indicate a stricture.
Treatment Options
The treatment for ureteral stricture depends on the severity and underlying cause. Common approaches include:
- Ureteral Dilation: This minimally invasive procedure uses a balloon or dilator to widen the narrowed segment.
- Stent Placement: A stent can be temporarily inserted into the ureter to maintain urine flow and relieve obstruction.
- Surgical Repair: In severe cases, reconstructive surgery such as ureteroplasty may be necessary to remove or bypass the stricture.
- Endoscopic Procedures: Techniques like laser ablation can break down scar tissue and restore ureteral function.
- Nephrostomy: In cases of severe obstruction, a tube may be placed through the skin to drain urine directly from the kidney.
Preventing Ureteral Strictures
While not all strictures are preventable, certain measures can reduce the risk:
- Prompt Treatment of UTIs: Early management prevents chronic inflammation that may lead to scarring.
- Hydration: Drinking plenty of water helps flush out potential irritants and reduces the risk of kidney stones.
- Monitoring After Surgery: Patients undergoing urinary tract procedures should be closely monitored for complications.
- Avoiding Trauma: Protecting the abdomen during physical activities reduces the risk of ureteral injuries.
Living with Ureteral Stricture
Living with a ureteral stricture requires regular follow-up care to monitor kidney function and prevent complications. Lifestyle adjustments, such as staying hydrated and avoiding activities that strain the abdomen, can support recovery. For those undergoing surgical or endoscopic treatment, adhering to post-procedure instructions is critical for successful outcomes.
Conclusion
Ureteral strictures can significantly impact urinary function and overall health, but timely diagnosis and appropriate treatment can restore normal urine flow and prevent long-term complications. By understanding the causes, symptoms, and treatment options, individuals can take proactive steps to address this condition and maintain a healthy urinary system. If you suspect symptoms of a ureteral stricture, consult a healthcare provider for a thorough evaluation and personalized care plan.

