Urethral Stricture
Understanding Urethral Stricture: Causes, Symptoms, and Treatment
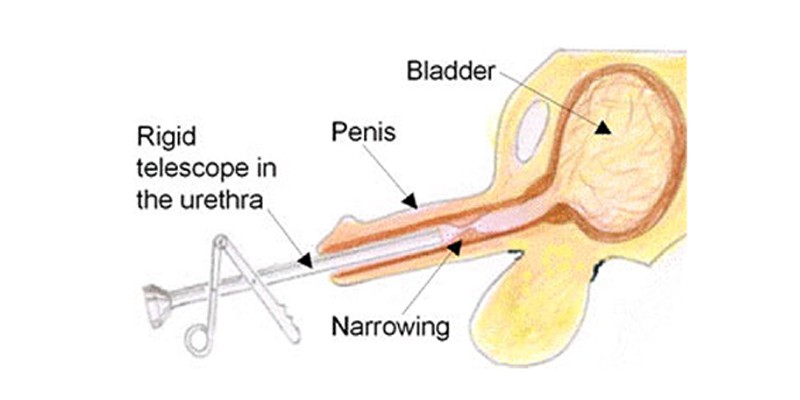
A urethral stricture is a narrowing of the urethra, the tube that carries urine from the bladder to the outside of the body. This condition can restrict the flow of urine, causing discomfort and potentially leading to severe complications if untreated. Urethral strictures can arise from various causes and present with distinctive symptoms, necessitating timely diagnosis and appropriate treatment.
What Causes Urethral Stricture?
Urethral strictures may develop due to several factors, including:
- Trauma: Injuries to the urethra, such as those sustained in accidents or during surgical procedures, can lead to scarring and narrowing.
- Infections: Recurrent urinary tract infections (UTIs) or sexually transmitted infections (STIs), such as gonorrhea, can result in inflammation and scarring of the urethra.
- Catheterization: Prolonged use or repeated insertion of urinary catheters can damage the urethra and cause strictures.
- Surgery: Procedures involving the prostate or urethra may result in scar tissue formation.
- Congenital Conditions: Some individuals are born with a naturally narrow urethra, which can worsen over time.
- Tumors: Growths in or around the urethra can compress the structure and lead to narrowing.
- Radiation Therapy: Treatments for pelvic cancers can damage urethral tissue, resulting in strictures.
Symptoms of Urethral Stricture
Symptoms of a urethral stricture vary based on the degree of narrowing and obstruction. Common signs include:
- Difficulty Urinating: A weak urine stream, straining to urinate, or incomplete bladder emptying.
- Frequent Urination: An increased urge to urinate, often with small amounts of urine passed.
- Pain or Discomfort: Burning sensation or pain during urination.
- Blood in Urine or Semen: This may result from irritation or damage to the urethra.
- Recurrent UTIs: Blockages caused by strictures increase the risk of infections.
- Urinary Retention: In severe cases, the urethra may become completely blocked, preventing urination.
Diagnosis
Diagnosing a urethral stricture typically involves a combination of medical history review, physical examination, and diagnostic tests:
- Medical History: The healthcare provider will inquire about symptoms, past infections, injuries, or surgeries involving the urinary tract.
- Physical Examination: A thorough examination may reveal signs of urinary retention or infection.
- Imaging Studies: Ultrasound, X-rays with contrast dye (retrograde urethrography), or cystoscopy provide detailed visuals of the urethra.
- Uroflowmetry: This test measures the speed and volume of urine flow, helping to identify blockages.
- Urine Tests: These can detect infections or the presence of blood.
Treatment Options
The treatment for urethral stricture depends on its severity, location, and underlying cause. Common treatments include:
- Dilation: A minimally invasive procedure where the urethra is gently stretched using specialized instruments.
- Urethrotomy: An endoscopic procedure in which a thin scope is used to cut the scar tissue and widen the urethra.
- Urethral Stent: In some cases, a stent may be placed to keep the urethra open.
- Open Surgery (Urethroplasty): In severe or recurrent cases, reconstructive surgery may be performed to remove or bypass the stricture.
- Catheterization: Temporary placement of a catheter can relieve urinary retention and allow the urethra to heal.
Preventing Urethral Strictures
While not all cases are preventable, certain practices can reduce the risk:
- Prompt Treatment of Infections: Early management of UTIs and STIs can prevent inflammation and scarring.
- Careful Catheter Use: Minimizing catheter use and ensuring proper insertion techniques reduce the risk of trauma.
- Protective Measures: Avoiding pelvic injuries through the use of protective gear during high-risk activities.
- Regular Medical Check-ups: Monitoring urinary symptoms and seeking medical attention promptly if issues arise.
Living with Urethral Stricture
Managing a urethral stricture often requires ongoing care and lifestyle adjustments. Regular follow-ups with a healthcare provider are crucial to monitor for recurrence or complications. Maintaining hydration, avoiding bladder irritants (such as caffeine and alcohol), and adhering to treatment plans can improve quality of life.
Conclusion
Urethral strictures can significantly impact urinary health and daily life, but effective treatments are available. Awareness of the symptoms and causes allows for early intervention, reducing the risk of complications such as urinary retention or kidney damage. If you experience symptoms of a urethral stricture, consult a healthcare provider for a thorough evaluation and personalized treatment plan. Timely care can restore normal urinary function and improve overall well-being.

